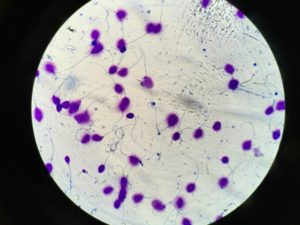
Semen Analysis:
The Andrology laboratory at Westlake IVF offers the most unique and thorough semen analysis. A semen sample can be collected by the male at home or at the Westlake IVF Andrology collection room. After the semen sample has been collected, the main parameters analyzed include volume of semen, concentration of sperm, motility, and morphology. After the semen sample has been analyzed, the report is reviewed and signed by our Reproductive Urologist.
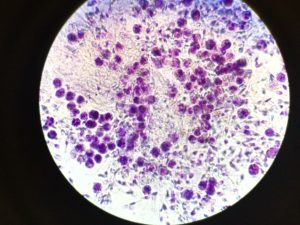 Seminal Leukocytes:
Seminal Leukocytes:
Along with a standard semen analysis all samples examined at the Andrology lab at Westlake IVF undergo an evaluation for leukocytes, or white blood cells. Leukocytes can look very similar to immature sperm cells so it is important to be able to differentiate between the 2 cell types, which is accomplished by using a special stain that allows differentiation between the 2 types. If there are a large number of leukocytes in the semen, this is an indicator of infection or inflammation which will need to be treated by the Reproductive Urologist to improve fertility potential.
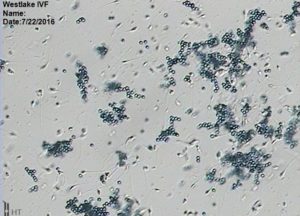 Antisperm Antibody testing:
Antisperm Antibody testing:
The Andrology laboratory at Westlake IVF offers a highly-specialized test called “Antisperm Antibody” testing. Sometimes, agglutination (also known as “clumping”) of sperm cells can be seen when the sample is visualized under the microscope. If the andrologist reports significant agglutination on the semen analysis report, then antisperm antibodies may be present and antisperm antibody testing may be recommended. There are 2 types of Antisperm Antibodies, IgA and IgG, which are from the immune system and may be attached to the head, midpiece, and/or tail of sperm and can potentially impact fertility.
Post-ejaculatory Urinalysis:
Some men will not have sperm in the semen due to a process known as retrograde ejaculation. This is when sperm go backwards into the bladder rather than out the urethra as they should, and they simply are urinated out with the man’s next voiding of his bladder. This may be seen in men with diabetes, spinal cord injuries, men who have had prostate surgery, are on specific medications, or have other potential risk factors for retrograde ejaculation. The andrologist at Westlake IVF assesses retrograde ejaculation by obtaining a urine sample immediately after orgasm and can identify sperm in the urine and can process the sperm to be used with assistance to help achieve a pregnancy when applicable.
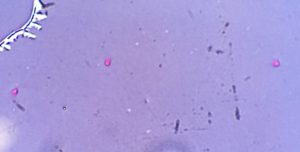 Viability Testing:
Viability Testing:
In certain circumstances a semen analysis may show sperm with zero motility, or sperm with no movement. In such cases, it is important to know if the sperm are actually viable to help understand their fertilizing potential with levels of assistance. A specialized viability test is performed in the situations to help elucidate the level of viability of the sperm.
Pentoxyifylline:
When sperm have no or low motility, they can be treated with an agent called Pentoxifylline, which can stimulate sperm motility. This is used to help identify the level of sperm viability as well as helping the andrologist/embryologist to select more viable sperm cells to use with levels of reproductive assistance.
 Sperm DNA Fragmentation Index (DFI):
Sperm DNA Fragmentation Index (DFI):
Although the traditional semen analysis parameters of semen volume, sperm concentration, motility, and morphology are certainly important in the assessment of a man’s fertility potential, they may be a relatively crude assessment. They do not tell us about the integrity of sperm’s DNA or its ability to fertilize an egg and maintain a pregnancy. At Westlake IVF, a highly specialized sperm DNA fragmentation index evaluation is being offered. This is a high level test revealing what percentage of sperm cells in a man’s semen have damaged DNA. When there is a high percentage of DNA damaged sperm, there are associations with lower fertilization and pregnancy rates and higher miscarriage rates. This test is being offered for select patients who have risk factors for having higher levels of DNA fragmentation and the need for this level of testing can be discussed in consultation with a Reproductive Urologist at Austin Fertility & Reproductive Medicine.
Viscosity Treatment:
In men with a high level of semen viscosity without a correctable cause for it, viscosity treatment may be recommended. This is especially useful in conjunction with treatment options such as IUI.
Sperm Cryopreservation:
Either ejaculated or surgically retrieved sperm may be frozen at Westlake IVF for future use.
Semen Preparation for Intrauterine Insemination (IUI):
The Andrology laboratory at Westlake IVF offers the clinical service of semen preparation for IUI. An IUI can be performed with a fresh or frozen semen sample. For IUI with a fresh semen sample, after the semen sample has been collected by the husband or male partner, the sample is processed by our andrologists inn preparation for the IUI. In the case of IUI with a frozen semen sample, the sample is thawed by our andrologists in preparation for the IUI.
Sperm Identification from PESA/TESE:
In men with no sperm in the semen due to an anatomic blockage, such as a vasectomy, percutaneous epididymal sperm extraction (PESA) or testicular sperm extraction (TESE) can be performed to retrieve sperm. This is performed by a Reproductive Urologist at Westlake IVF in the sperm retrieval suite adjacent to the IVF laboratory with a minimally invasive technique. The andrologist/embryologist assesses the sperm retrieved for use or for cryopreservation for future use.
Sperm Identification from Microdissection Testicular Sperm Extraction:
In cases of nonobstructive azoospermia (NOA), in which a male does not have sperm cells in his seminal fluid due to inadequate sperm production, not due to a blockage, but may have some small pockets of sperm cells within the testicle, a surgery known as Microdissection Testicular Sperm Extraction (microTESE) may be performed by a fellowship-trained Reproductive Urologist. This surgery involves the removal of small biopsies of testicular tissue in the Operating Room; our embryologists accompany our Reproductive Urologist in the Operating Room and are able to evaluate the testicular tissue under a high-powered microscope at that time in the Operating Room. Sperm obtained through this process can be used in conjunction with invitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) to help couples in this challenging situation conceive.


